Understanding Temporomandibular (TMJ) Pain: Causes, Symptoms, and Relief
After over a decade of working with clients at Revive Massage Therapy, I've seen firsthand how debilitating temporomandibular (TMJ) pain can be. What often starts as a slight clicking in the jaw or occasional discomfort can escalate into chronic pain that affects every aspect of daily life—from enjoying a meal to getting a good night's sleep.
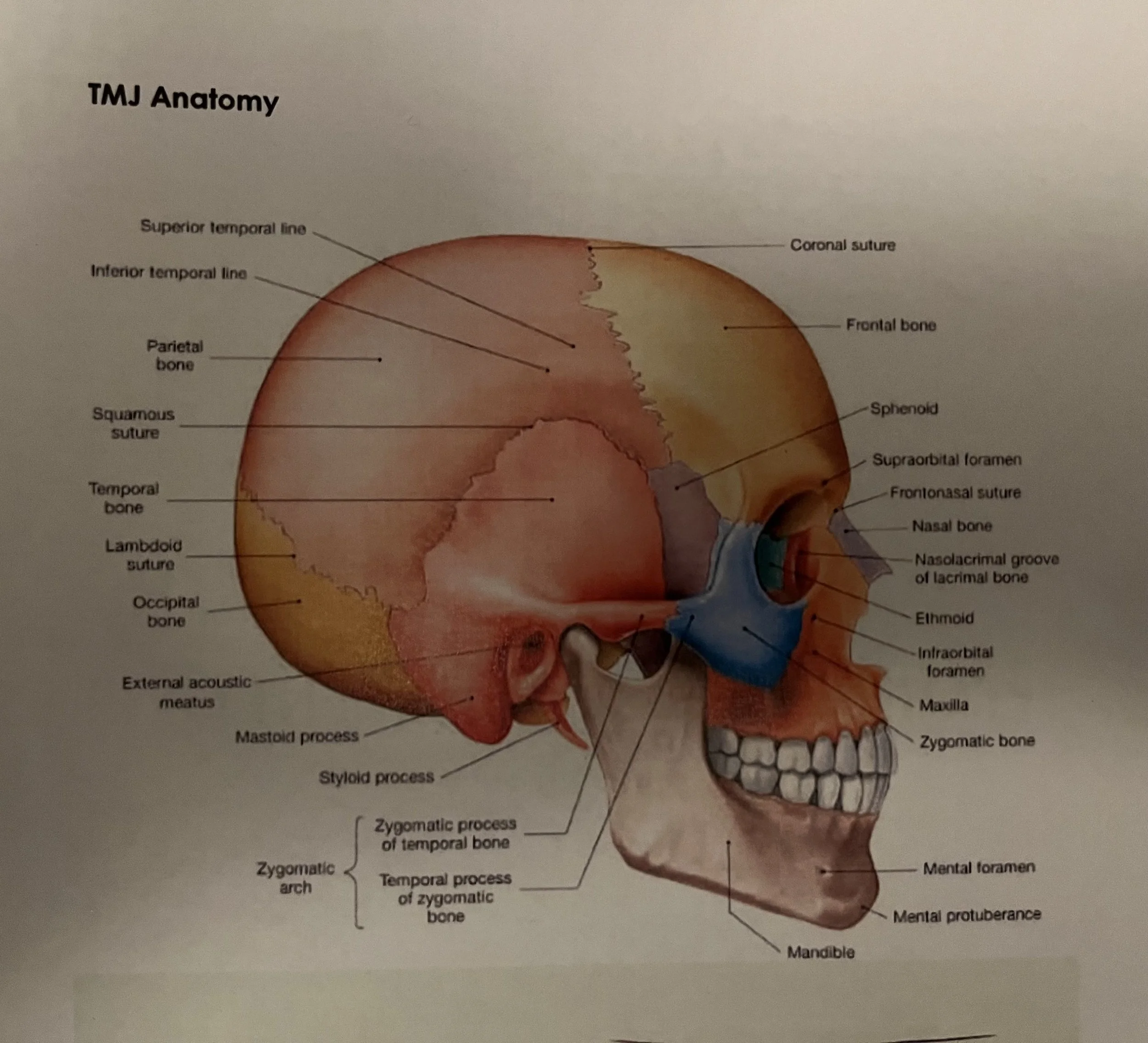
TMJ Anatomy
What is the Temporomandibular Joint?
The temporomandibular joint (TMJ) connects your jawbone to your skull, functioning as a sliding hinge on each side of your jaw. It's one of the most complex and frequently used joints in the body, allowing for both rotational and translational movements necessary for chewing, speaking, and yawning.
When this intricate system becomes dysfunctional, the resulting Temporomandibular Disorder (TMD) can create a cascade of symptoms throughout the head, neck, and shoulders.
The second most common musculoskeletal disorders in adults are Temporomandibular Disorders (TMD) and are responsible for significant pain and disability with approximately 33% of adults reporting at least one symptom of TMD dysfunction*1
Recognising the Symptoms
The symptoms can often extend far beyond the jaw itself:
Jaw pain or tenderness around the joint area, often worse in the morning or after periods of stress
Clicking, popping, or grinding sounds when opening or closing the mouth
Limited jaw movement or the uncomfortable sensation of jaw locking
Facial pain that radiates into the neck and shoulders
Persistent headaches and earaches that don't respond to typical treatments
Difficulty chewing or discomfort while eating, particularly with harder foods
Chronic muscle tension in the face, neck, and shoulders
Many of my clients initially don't connect their shoulder tension or headaches to their jaw—they're often surprised to learn these symptoms are related.
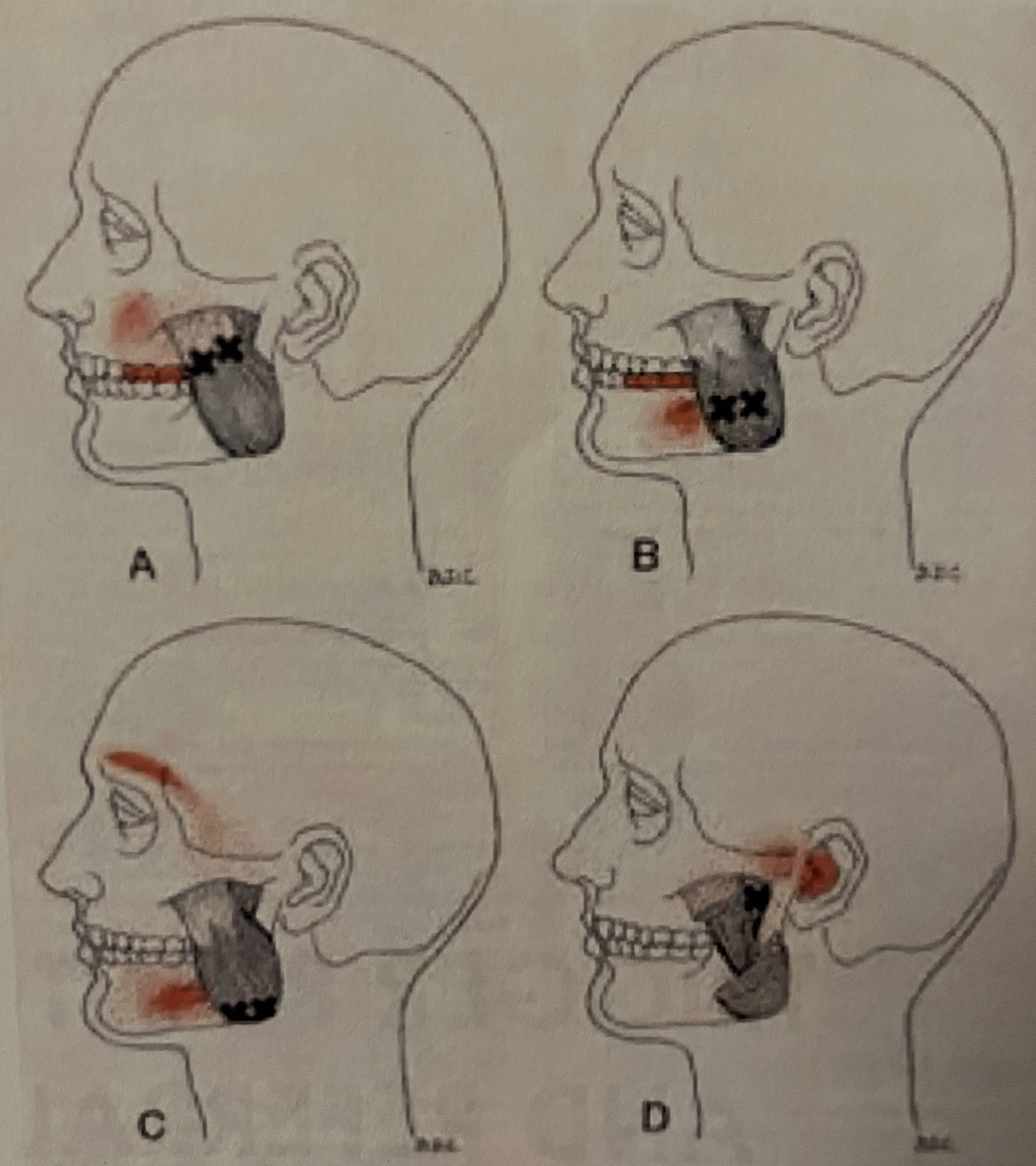
Some trigger point pain patterns of the TMJ
Causes of TMJ Pain?
Through my work, I've observed that TMJ pain rarely has a single cause. Instead, it typically develops from a combination of factors:
Physical Factors:
Teeth grinding (bruxism) or jaw clenching, particularly during sleep or periods of concentration
Arthritis affecting the jaw joint
Previous jaw injury or trauma, even from years ago
Misaligned bite or dental problems
Structural imbalances in the neck and upper back
Lifestyle and Stress Factors:
Chronic stress leading to unconscious jaw clenching—something I see constantly in my desk-working clients
Poor posture, especially forward head posture from computer work
Excessive gum chewing or habits like nail biting or pen chewing
Prolonged jaw positioning during lengthy dental procedures
The Desk Worker Connection
Given that the majority of my clients are women aged 30-60 who work at desks, I've noticed a strong correlation between poor ergonomics, forward head posture, and TMJ pain. When your head shifts forward—as it often does during computer work—the muscles at the back of your neck must work harder to support it. This creates a chain reaction: neck tension leads to shoulder tension, which affects the muscles that attach to the jaw, ultimately contributing to TMJ dysfunction*2
Treatment and Management: A Holistic Approach
Effective management requires addressing the whole person, not just the jaw. This is where my Advanced Clinical Massage training becomes invaluable.
Professional Treatment:
At Revive Massage Therapy, I use advanced techniques including deep tissue work, trigger point therapy, myofascial release, and stretching to address the muscular component of TMJ pain. This involves working not just on the jaw itself, but on the entire kinetic chain—the neck, shoulders, upper back, and even the chest muscles that influence head and jaw position.
Image © Jing Massage
The Fix in Six Programme for TMJ Pain
For clients experiencing TMJ pain, I often recommend my Fix in Six programme—a structured series of six treatments designed specifically for pain relief and functional improvement.
TMJ pain, like most chronic pain conditions, doesn't develop overnight, and it won't resolve with a single treatment. The body needs time to unlearn compensatory patterns and allow the nervous system to calm down. This is particularly true when the sympathetic nervous system has been overactive due to chronic pain and stress.
The Fix in Six programme works because:
Consistency matters: Regular treatments allow us to progressively release deep-seated tension
Pattern interruption: Multiple sessions help break the cycle of muscle guarding and pain
Nervous system regulation: Repeated therapeutic touch helps shift the body from a stressed state to a healing state
Accountability: A structured programme keeps you committed to your recovery
Comprehensive approach: We address not just the jaw, but all contributing factors including posture, stress, and compensatory patterns
Many clients who complete the Fix in Six programme for TMJ pain report significant improvements*4 in jaw mobility, reduced clicking and popping, fewer headaches, and better sleep quality.
Self-Care Strategies:
Apply ice during acute flare-ups to reduce inflammation, then use heat therapy for chronic muscle tension
Practice gentle jaw exercises and stretching (I provide these to clients during treatment)
Maintain good posture throughout the day, especially at your workspace
Avoid hard, chewy, or tough foods during painful episodes
Practice stress management techniques like meditation or breathwork
Be mindful of jaw clenching during the day—set reminders to check in with your jaw position
Image © Revive Therapy
My Specialised Approach
I have recently completed specialised TMJ training, building on my BTEC Level 6 Diploma in Advanced Clinical Massage and Sports Therapy—the highest qualification available in the UK and Europe. This additional training allows me to offer even more targeted, effective treatment for temporomandibular disorders.
My approach involves:
Detailed assessment of jaw mechanics, posture, and movement patterns
Intra-oral and extra-oral massage techniques to address the muscles of mastication
Treatment of the neck, shoulders, and upper back to address contributing factors
Education on self-care exercises and ergonomic improvements
Collaboration with your dentist or other healthcare providers when appropriate
When to Seek Professional Help
Don't wait until the pain becomes unbearable. Consult a healthcare professional if you experience:
Persistent jaw pain lasting more than a few days
Difficulty opening your mouth wide
Jaw locking, catching, or deviating to one side
Severe headaches associated with jaw pain
Symptoms that interfere with eating, speaking, or sleeping
Progressive worsening of symptoms
Prevention: The Best Medicine
Based on my years of experience, here are my top recommendations for preventing TMJ pain:
Mind your posture: Set up your workspace ergonomically and take regular breaks
Manage stress proactively: Don't wait until you're overwhelmed—build stress management into your daily routine
Notice jaw clenching: Throughout the day, check in with your jaw—your teeth shouldn't be touching except when eating
Avoid excessive jaw movements: Be mindful of wide yawning, gum chewing, or biting into very hard foods
Consider a night guard: If you grind your teeth at night, speak to your dentist about a custom guard
Regular maintenance treatments: Even after pain resolves, periodic massage helps prevent recurrence
A Condition That Responds to Care
The good news is that TMJ pain is highly treatable. In my practice, I've seen countless clients find relief and regain quality of life through a combination of skilled manual therapy, self-care strategies, and addressing underlying lifestyle factors.
If you're experiencing jaw pain, clicking, or any of the symptoms described here, know that you don't have to live with it. With proper understanding, professional treatment, and commitment to your own care, most people achieve significant improvement.
References:
1. Mnguni, Nkazimulo1; Olivier, B., Mosselson, J. Prevalence of concurrent headache and temporomandibular disorders: a systematic review protocol; JBI Evidence Synthesis, 19(1), pp. 263–269. https://doi.org/10.11124/jbisrir-d-19-00255.
2. Sambataro S, Cervino G, Bocchieri S, La Bruna R, Cicciù M. TMJ Dysfunctions Systemic Implications and Postural Assessments: A Review of Recent Literature. J Funct Morphol Kinesiol. 2019 Aug 19;4(3):58. doi: 10.3390/jfmk4030058. PMID: 33467373; PMCID: PMC7739223.
3. Gębska M, Dalewski B, Pałka Ł, Kołodziej Ł. Evaluation of the efficacy of manual soft tissue therapy and therapeutic exercises in patients with pain and limited mobility TMJ: a randomized control trial (RCT). Head Face Med. 2023 Sep 8;19(1):42. doi: 10.1186/s13005-023-00385-y. PMID: 37684652; PMCID: PMC10486124.
4. Clarke, N Evaluating the Effects of the Jing Method on Temporomandibular Joint (TMJ) Pain in People aged 25 – 65 years of age. 2024